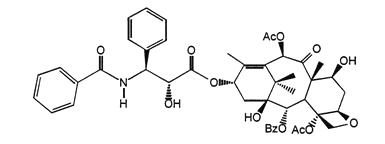
Paclitaxel
What is Abraxane (Paclitaxel)?
Approved To Treat
Related Clinical Trials
Summary: This phase II/III trial compares the addition of radiation therapy to the usual treatment (immunotherapy with or without chemotherapy) versus (vs.) usual treatment alone in treating patients with non-small cell lung cancer that may have spread from where it first started to nearby tissue, lymph nodes, or distant parts of the body (advanced) or that has spread from where it first started (primary s...
Summary: This phase III ALCHEMIST treatment trial tests the addition of pembrolizumab to usual chemotherapy for the treatment of stage IIA, IIB, IIIA or IIIB non-small cell lung cancer that has been removed by surgery. Immunotherapy with monoclonal antibodies, such as pembrolizumab, may help the body's immune system attack the cancer, and may interfere with the ability of tumor cells to grow and spread. Ch...
Summary: The purpose of this study is to compare the clinical benefit of the combination of BMS-986504 (a selective MTA-cooperative inhibitor of PRMT5) plus pembrolizumab and chemotherapy versus placebo plus pembrolizumab and chemotherapy in first-line metastatic non-small cell lung cancer participants with homozygous MTAP deletion
Related Latest Advances
Brand Information
- Do not administer ABRAXANE therapy to patients with baseline neutrophil counts of less than 1,500 cells/mm
- Monitor for neutropenia, which may be severe and result in infection or sepsis
- Perform frequent complete blood cell counts on all patients receiving ABRAXANE
- Baseline neutrophil counts of < 1,500 cells/mm
- A history of severe hypersensitivity reactions to ABRAXANE
Neutropenia was dose dependent and reversible. Among patients with metastatic breast cancer in the randomized trial, neutrophil counts declined below 500 cells/mm3 (Grade 4) in 9% of the patients treated with a dose of 260 mg/m2 compared to 22% in patients receiving paclitaxel injection at a dose of 175 mg/m2. Pancytopenia has been observed in clinical trials.
Infectious episodes were reported in 24% of the patients treated with ABRAXANE. Oral candidiasis, respiratory tract infections and pneumonia were the most frequently reported infectious complications.
Grade 1 or 2 HSRs occurred on the day of ABRAXANE administration and consisted of dyspnea (1%) and flushing, hypotension, chest pain, and arrhythmia (all <1%). The use of ABRAXANE in patients previously exhibiting hypersensitivity to paclitaxel injection or human albumin has not been studied.
Hypotension, during the 30-minute infusion, occurred in 5% of patients. Bradycardia, during the 30-minute infusion, occurred in <1% of patients. These vital sign changes most often caused no symptoms and required neither specific therapy nor treatment discontinuation.
Dyspnea (12%), cough (7%), and pneumothorax (<1%) were reported after treatment with ABRAXANE.
The frequency and severity of sensory neuropathy increased with cumulative dose. Sensory neuropathy was the cause of ABRAXANE discontinuation in 7/229 (3%) patients. Twenty-four patients (10%) treated with ABRAXANE developed Grade 3 peripheral neuropathy; of these patients, 14 had documented improvement after a median of 22 days; 10 patients resumed treatment at a reduced dose of ABRAXANE and 2 discontinued due to peripheral neuropathy. Of the 10 patients without documented improvement, 4 discontinued the study due to peripheral neuropathy.
Ocular/visual disturbances occurred in 13% of all patients (n=366) treated with ABRAXANE and 1% were severe. The severe cases (keratitis and blurred vision) were reported in patients who received higher doses than those recommended (300 or 375 mg/m2). These effects generally have been reversible.
The symptoms were usually transient, occurred two or three days after ABRAXANE administration, and resolved within a few days.
Grade 3 or 4 elevations in GGT were reported for 14% of patients treated with ABRAXANE and 10% of patients treated with paclitaxel injection in the randomized trial.
Overall 11% of patients experienced creatinine elevation, 1% severe. No discontinuations, dose reductions, or dose delays were caused by renal toxicities.
Nail changes (changes in pigmentation or discoloration of nail bed) have been reported. Edema occurred in 10% of patients; no patients had severe edema. Dehydration and pyrexia were also reported.